Patient Instructions
Pre and Post Treatment instructions
Welcome to Pioneer Vein Clinic’s patient instruction page! We’re dedicated to providing a stress-free, valuable experience, and we know that being prepared is an important first step. Please browse the patient instructions that meet your needs, and feel free to contact us with any questions!
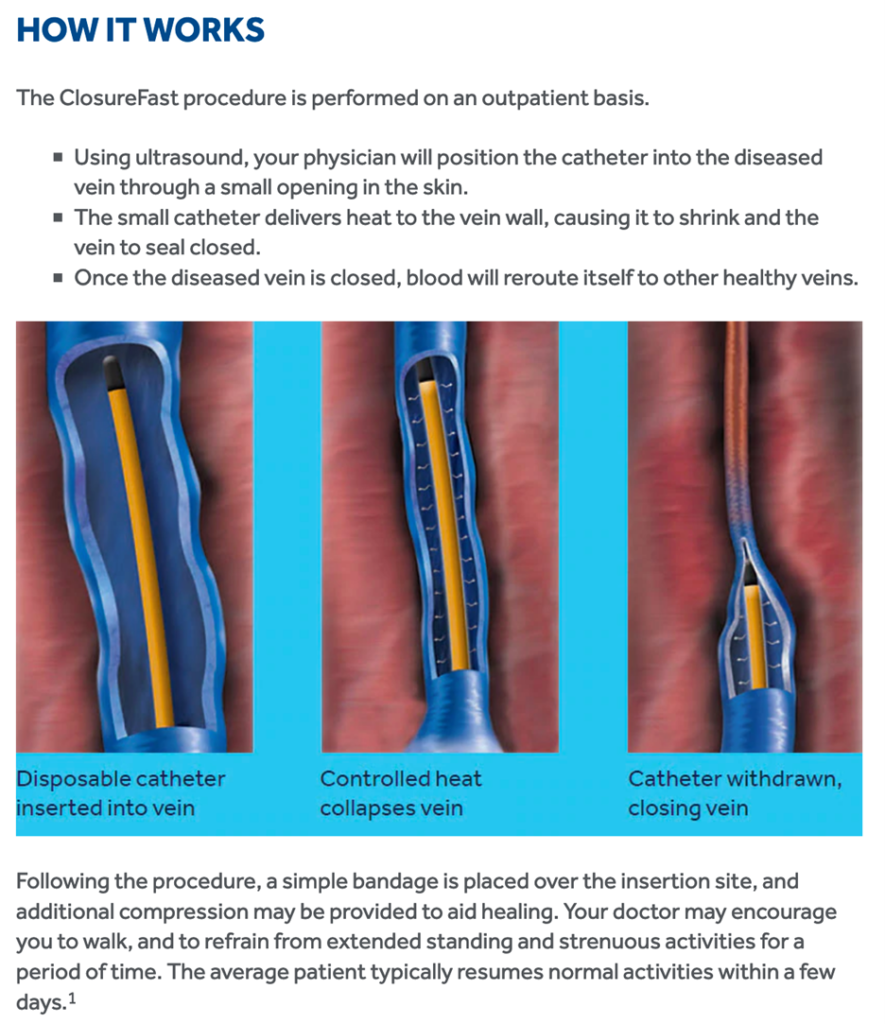
Radiofrequency Ablation (ClosureFast)
Pre-Procedure Instructions
- Fill all procedure-related prescriptions PRIOR to your surgery. (For example: compression stockings)
- No compression wraps/hose 48 hours prior to procedure
- Bring your insurance card, photo identification and medical device card(s) if applicable with you
- Bring a copy of your healthcare power of attorney/Advance Directive/Living Will with you
- You are NOT required to schedule a pre-op visit with your family physician prior to your cardiac procedure
For Sedation Patients:
- Alcohol should NOT be consumed for 24 hours prior to and after your procedure
- Assign a trusted person to drive you home after you are cleared to be released
The Morning of Your Procedure:
- Do not eat for 5 hours prior to your procedure
- Shower with antibacterial soap
- Wear comfortable, loose clothing
- You can wear contact lenses, if you prefer
- Check to make sure you have brought compression stocking with you
- If you would like to listen to music, you may bring a personal device with headphones
- Notify the office first thing, should you develop a cold or other symptoms prior to surgery
Medications:
Bring ALL your medications with you in the original containers (including inhalers, eye drops and Insulin).
UNLESS YOUR PHYSICIAN HAS ADVISED YOU OTHERWISE…
- Take any of your regular medication as directed
- Continue Coumadin, Aspirin, Plavix, Xarelto, Eliquis and other blood thinners as normal
- Hold water pills the morning of procedure
- Hold oral diabetic medications the morning of the procedure
- Decrease long acting insulin dose by one third the night before
- Hold insulin dose the morning of the procedure
- Bring your CPAP machine including the mask and tubing
Procedure Day
After check in you will be taken to your room, the nurse will review your history, measure your vital signs and complete the consent forms. You will be given a hospital gown to wear. After that you may be given a mild oral sedative such as Ativan or Valium. In some cases, Intravenous sedation may be given. An IV will be placed in your arm if IV sedation is planned.
The Sonographer under your physician’s guidance will then map the vein to be treated. The affected limb will be painted with an antiseptic such as iodine or chlorhexidine and draped.
After administering a local anesthetic, your physician will insert a small needle at an appropriate spot and place a catheter in the vein to be treated. Under ultrasound a tumescent solution of saline with an anesthetic and epinephrine is injected at multiple spots along and around the vein. Radiofrequency is then applied using the catheter along the entire length of the vein. Typically, this is not painful.
After the ablation, the treated limb is wrapped with gauze and elastic bandage.
The entire procedure takes around one hour.
Post-Procedure Instructions
DAY OF PROCEDURE:
DRESSING:
- Post procedure your leg will be wrapped with a cotton gauze/ACE compression dressing
- The wrap will be tight and firm but should NOT be uncomfortably tight. If it is uncomfortably tight you should unwrap the ACE bandage, leave the cotton wrap in place, and re-wrap the ACE to your comfort.
- Uncommonly, you may see some evidence of bloody drainage on the wrap. If it appears to be enlarging, you should lie down, elevate your leg (foot above the level of your heart) and apply pressure over the area. If this does not stop bleeding after a short time (20 to 30 minutes) notify Pioneer Vein Center Physician.
ACTIVITY:
- Walk for at least 20 min
- When sitting keep your leg elevated
- Do not drive if you have received any sedation
- See below for additional instructions
MEDICATIONS:
- Resume all your home medications the same day of your procedure
- Resume your Anticoagulants such as Coumadin, Xarelto, Eliquis, Brilinta, Plavix etc. UNLESS YOU PHYSICIAN HAS ADVISED YOU OTHERWISE
POST PROCEDURE WEEK:
BATHING:
- You may shower the day after the procedure
- Do not soak in a bath for 72 hours
COMPRESSION:
- After showering, put on the compression hose. Compression will either be provided at the office or a prescription for hose will be given. The compression hose needs to be worn continuously (including at night) for the next 24 hours.
- For the following 2 weeks wear the compression stockings during the day
ACTIVITY & EXERCISE:
- It is important that you walk for at least 20 minutes per day after this procedure, although an hour per day is preferred
- Light exercise like bike riding or gentle aerobics are safe options after 48 hours
- Vigorous exercises, bearing down, squatting, heavy weightlifting (>40LB) should be avoided for one week
PAIN:
- Manageable amounts of tenderness, bruising, and inflammation is expected after this procedure. It is also common for tenderness to increase slightly during your second week of recovery. These symptoms can be safely relieved with the use of over the counter ibuprofen (Advil), acetaminophen (Tylenol), and naproxen (Aleve).
FOLLOW UP:
- You will come in within a week (Usually 2 to 3 days) of each procedure for an ultrasound and wound check
- After your final procedure, we will ask you to come in for a follow up appointment around six weeks later
IMMEDIATELY CALL PIONEER VEIN CENTER OFFICE IF YOU EXPERIENCE:
- Warmth or redness along the treated portion
- Fever over 101ºF
- Prolonged tenderness
- Shortness of breath
- Swelling in the treated limb
- Moderate or severe pain that stop you from performing normal activities
- Bleeding that cannot be controlled with moderate pressure
- Please feel free to call with any other questions or concerns
Adhesive Ablation (Venaseal)
Pre-Procedure Instructions
- Fill all procedure-related prescriptions PRIOR to your surgery (for example: compression stockings)
- No compression wraps/hose 48 hours prior to procedure
- Bring your insurance card and photo identification with you
- Bring a copy of your healthcare power of attorney/Advance Directive/Living Will with you
- You are NOT required to schedule a pre-op visit with your family physician prior to your cardiac procedure
For Sedation Patients:
- Alcohol should NOT be consumed for 24 hours prior to and after your procedure
- Assign a trusted person to drive you home after you are cleared to be released
The Morning of Your Procedure:
- Do not eat for 5 hours prior to your procedure
- Shower with antibacterial soap
- Wear comfortable, loose clothing
- You can wear contact lenses, if you prefer
- Check to make sure you have brought compression stocking with you
- If you would like to listen to music, you may bring a personal device with headphones
- Notify the office first thing, should you develop a cold or other symptoms prior to surgery
Medications:
Bring ALL your medications with you in the original containers (including inhalers, eye drops and Insulin)
UNLESS YOUR PHYSICIAN HAS ADVISED YOU OTHERWISE…
- Take any of your regular medication as directed
- Continue Coumadin, Aspirin, Plavix, Xarelto, Eliquis and other blood thinners as normal
- Hold water pills the morning of procedure
- Hold oral diabetic medications the morning of the procedure
- Decrease long acting insulin dose by one third the night before
- Hold insulin dose the morning of the procedure
- Bring your CPAP machine including the mask and tubing
Procedure Day
After check in you will be taken to your room, the nurse will review your history, measure your vital signs and complete the consent forms. You will be given a hospital gown to wear. After that you may be given a mild oral sedative such as Ativan or Valium. In some cases, Intravenous sedation may be given. An IV will be placed in your arm if IV sedation is planned.
The Sonographer under your physician’s guidance will then map the vein to be treated. The affected limb will be painted with an antiseptic such as iodine or chlorhexidine and draped.
After administering a local anesthetic, your physician will insert a small needle and place a sheath in the vein. Using Ultrasound guidance, a delivery catheter is placed at the desired area. A special proprietary formulation of the surgical glue (VenaSeal™) is administered and pressure applied over the area. The catheter is then pulled back and more glue is administered in the same manner until the entire vein is treated. A Band-Aid is placed at the site of entry.
The entire procedure takes about an hour.
Post-Procedure Instructions
DAY OF PROCEDURE:
DRESSING
- Post procedure a Band-Aid or Coban dressing will be placed at the site of needle entry
- Uncommonly, you may see some evidence of bloody drainage on the wrap/Band-Aid. If it appears to be enlarging, you should lie down, elevate your leg (foot above the level of your heart) and apply pressure over the area. If this does not stop bleeding after a short time (20 to 30 minutes) notify Pioneer Vein Center Physician.
ACTIVITY:
- Resume normal activities
- Walk for at least 20 min
- When sitting keep your leg elevated
- Do not drive if you have received any sedation
- See below for additional instructions
MEDICATIONS:
- Resume all your home medications the same day of your procedure
- Resume your Anticoagulants such as Coumadin, Xarelto, Eliquis, Brilinta, Plavix etc. UNLESS YOU PHYSICIAN HAS ADVISED YOU OTHERWISE
POST PROCEDURE WEEK:
BATHING:
- You may shower the day after the procedure
- Do not soak in a bath for 72 hours after the procedure
COMPRESSION:
- You are not required to but may use your compression stockings during the day. Some patients report improved comfort with the stockings.
ACTIVITY & EXERCISE:
- It is important that you walk for at least 20 minutes every day after this procedure, although an hour per day is preferred
- Light exercise like bike riding or gentle aerobics are safe options
- Vigorous exercises, bearing down, squatting, heavy weightlifting (>40LB) should be avoided for one week
- When sitting keep your leg elevated
PAIN and SIDE EFFECTS:
- Manageable amounts of tenderness, bruising, and inflammation is expected after this procedure. It is also common for tenderness to increase slightly during your second week of recovery. These symptoms can be safely relieved with the use of over the counter ibuprofen (Advil), acetaminophen (Tylenol), and naproxen (Aleve).
- Erythema (Redness), Itching, Pain, Edema, tenderness over the treated vein may occur 7 to 14 days after the procedure. This usually resolves within a week.
- If painful you may take over the counter ibuprofen (Advil), acetaminophen (Tylenol), and naproxen (Aleve)
- Anti-inflammatory cream such as diclofenac 1%(Voltaren) cream may be applied over the area
- If Itching is present Benadryl may be taken (Benadryl can cause sedation)
- Please CALL our office for proper guidance for treatment of these symptoms
- You may feel a cord over the area of your treated vein. This usually softens over few weeks.
FOLLOW UP:
- You will come in within a week (Usually 2 to 3 days) of each procedure for an ultrasound and wound check
- After your final procedure, we will ask you to come in for a follow up appointment around six weeks later
IMMEDIATELY CALL PIONEER VEIN CENTER OFFICE IF YOU EXPERIENCE:
- Warmth or redness along the treated portion
- Fever over 101ºF
- Prolonged tenderness
- Shortness of breath
- Swelling in the treated limb
- Moderate or severe pain that stop you from performing normal activities
- Bleeding that cannot be controlled with moderate pressure
- Please feel free to call with any other questions or concerns
Sclerotherapy
Pre-Procedure Instructions
- No compression wraps/hose 48 hours prior to procedure
- Bring your insurance card and photo identification with you
- Bring a copy of your healthcare power of attorney/Advance Directive/Living Will with you
- You are NOT required to schedule a pre-op visit with your family physician prior to your cardiac procedure
Pre-Procedure Instructions
- Fill all procedure-related prescriptions PRIOR to your surgery such as Compression stockings and bring them with you
- Do not shave or use lotion on your legs the day of the procedure
- Discontinue use of artificial tanner at least one week prior to the procedure
- We recommend that you avoid iron supplements around the time of your procedure
For Sedation Patients:
- Sedation is generally not administered, however if sedation is planned then:
- Alcohol should NOT be consumed for 24 hours prior to and after your procedure
- Assign a trusted person to drive you home after you are cleared to be released
The Morning of Your Procedure:
- If you are receiving sedation do not eat for 5 hours prior to your procedure
- Shower with antibacterial soap
- Wear comfortable, loose clothing
- You can wear contact lenses, if you prefer
- Check to make sure you have brought compression stocking with you
- If you would like to listen to music, you may bring a personal device with headphones
- Notify the office first thing, should you develop a cold or other symptom prior to surgery
Medications:
Bring ALL your medications with you in the original containers (including inhalers, eye drops and Insulin)
UNLESS YOUR PHYSICIAN HAS ADVISED YOU OTHERWISE…
- Take any of your regular medication as directed
- Continue Coumadin, Aspirin, Plavix, Xarelto, Eliquis and other blood thinners as normal
- Hold water pills the morning of procedure
- Hold oral diabetic medications the morning of the procedure
- Decrease long acting insulin dose by one third the night before
- Hold insulin dose the morning of the procedure
- Bring your CPAP machine including the mask and tubing
Procedure Day
After check in you will be taken to your room, the nurse will review your history, measure your vital signs and complete the consent forms. Photographs of the affected area will be taken. You will be given a hospital gown or shorts to wear. After that you may be given a mild oral sedative such as Ativan or valium.
The affected limb will be painted with an antiseptic such as chlorhexidine and draped.
Using vein illuminating lights, your physician will insert a very tiny needle into the spider vein and inject the sclerosant Polidocanol (AscleraTM). This process is repeated until the desired area is treated. Multiple areas may require additional treatment sessions. If the extent of veins needing treatment requires ≥10 ml maximum dose of Polidocanol per session, repeat treatments separated by 1 to 2 weeks may be necessary.
After the ablation compression with an elastic bandage or stocking is applied. You will be observed for 30 min after the procedure for possible severe (anaphylactic) allergic reaction.
The entire procedure takes around one hour.
Post-Procedure Instructions
DAY OF PROCEDURE:
DRESSING:
- We ask that you continuously leave any wraps, tape, and/or compression stockings on continuously for 48hrs after sclerotherapy
ACTIVITY:
- Resume Normal activities
- Walk for at least 20 min
- When sitting keep your leg elevated
- Do not drive if you have received any sedation
- See below for additional instructions
MEDICATIONS:
- Resume all your home medications the same day of your procedure
- Resume your Anticoagulants such as Coumadin, Xarelto, Eliquis, Brilinta, Plavix etc. UNLESS YOU PHYSICIAN HAS ADVISED YOU OTHERWISE
POST PROCEDURE WEEK:
BATHING:
- The second morning after your sclerotherapy procedure, you can shower, leaving the stockings on. After your shower, you may lie down in bed in order to switch into dry stockings
- We recommend avoiding saunas, hot tubs, and any extended exposure to heat-based therapies that risk dilation of the blood vessels for two weeks
- No Sunbathing for one week
COMPRESSION:
- We ask that you continuously leave any wraps, tape, and/or compression stockings on continuously for 48hrs after sclerotherapy.
- After the first 2 nights, you wear them only during the day for 2 to 3 weeks.
ACTIVITY & EXERCISE:
- It is important that you walk for at least 20 minutes per day after this procedure, although an hour per day is preferred for 2 to 3 weeks
- Light exercise like bike riding or gentle aerobics are safe options.
- Vigorous exercise Valsalva maneuvers, squatting, heavy weightlifting (≥ 40LB), or any activity that requires you to “bear down” should be avoided for two weeks.
- Avoid long flight and car journey for 1 week
- Avoid wearing high heals
PAIN:
- Manageable amounts of tenderness, irritation, bruising, and inflammation is expected after this procedure. It is also common for tenderness to increase slightly during your second week of recovery.
- These symptoms can be safely relieved with the use of ibuprofen (Advil), acetaminophen (Tylenol), and naproxen (Aleve).
FOLLOW-UP:
- We will schedule a follow up appointment around two months following your final sclerotherapy session, so that we may evaluate results and determine if more sclerotherapy is required.
- Multiple treatments, 1 to 3 are typical. Repeat treatments are generally separated by 1-2 weeks.
SIDE EFFECTS:
- Irritation, Bruising, Itching and pain:
- Resolves with time
- Intravenous Thrombi:
- There are times when blood gets trapped inside a vein, and can be removed by micro-thrombectomy
- Hyperpigmentation:
- One of the most common side-effects experienced after sclerotherapy is a dark, reddish-brown change in the skin along the injection sites
- This change can take months or years to fully resolve, and in some situations can be permanent
- Hyperpigmentation happens as a result of iron deposition from trapped red blood cells in the treated area.
- We recommend that you avoid iron supplements around the time of your procedure in order to reduce the chances of this condition.
IMMEDIATELY CALL PIONEER VEIN CENTER IF YOU EXPERIENCE:
- Warmth or redness along the treated portion
- Fever over 101ºF
- Prolonged tenderness
- Shortness of breath
- Swelling in the treated limb
- Moderate or severe pain that stop you from performing normal activities
- Infection or inflammation
- Visible, superficial clots to treated areas
- Please also feel free to call with any questions or concerns
Phlebectomy
Pre-Procedure Instructions
- Fill all procedure-related prescriptions PRIOR to your surgery. (For example: compression stockings)
- No compression wraps/hose 48 hours prior to procedure
- Bring your insurance card and photo identification with you
- Bring a copy of your healthcare power of attorney/Advance Directive/Living Will with you
- You are NOT required to schedule a pre-op visit with your family physician prior to your cardiac procedure
For Sedation Patients:
- Alcohol should NOT be consumed for 24 hours prior to and after your procedure
- Assign a trusted person to drive you home after you are cleared to be released
The Morning of Your Procedure:
- Do not eat for 5 hours prior to your procedure
- Shower with antibacterial soap
- Wear comfortable, loose clothing
- You can wear contact lenses, if you prefer
- Check to make sure you have brought compression stocking with you
- If you would like to listen to music, you may bring a personal device with headphones
- Notify the office first thing, should you develop a cold or other symptoms prior to surgery
Medications:
Bring ALL your medications with you in the original containers (including inhalers, eye drops and Insulin)
UNLESS YOUR PHYSICIAN HAS ADVISED YOU OTHERWISE…
- Take any of your regular medication as directed
- If you are on a blood thinner, ask your physician if it needs to be discontinued
- Hold water pills the morning of procedure
- Hold oral diabetic medications the morning of the procedure
- Decrease long acting insulin dose by one third the night before
- Hold insulin dose the morning of the procedure
- Bring your CPAP machine including the mask and tubing
Procedure Day
Your physician will then map and mark the vein to be treated. The limb will be painted with an antiseptic such as iodine or chlorhexidine and draped.
A tumescent anesthesia solution of saline with an anesthetic and epinephrine is injected at multiple spots along and varicose veins. Small nicks will be made alongside of the vein and the vein is avulsed through its opening in segments. Small steri-strips are placed across the nicks and the limb is wrapped with gauze and elastic bandage.
The entire procedure takes around one hour.
Post-Procedure Instructions
DAY OF PROCEDURE:
DRESSING:
- Post procedure your leg will be wrapped with a cotton/ACE compression dressing
- The wrap will be tight and firm but should NOT be uncomfortably tight. If it is uncomfortably tight you should unwrap the ACE bandage, leave the cotton wrap in place, and re-wrap the ACE to your comfort.
- Uncommonly, you may see some evidence of bloody drainage on the wrap. If it appears to be enlarging, you should lie down, elevate your leg (foot above the level of your heart) and apply pressure over the area. If this does not stop bleeding after a short time (20 to 30 minutes) notify Pioneer Heart Vein Clinic physician
ACTIVITY:
- Resume normal activities
- Walk for at least 20 min
- When sitting keep your leg elevated
- Do not drive if you have received any sedation
- See below for additional instructions
MEDICATIONS:
- Resume all your home medications the same day of your procedure
- Resume your Anticoagulants such as Coumadin, Xarelto, Eliquis, Brilinta, Plavix etc. UNLESS YOUR PHYSICIAN HAS ADVISED YOU OTHERWISE
POST-PROCEDURE WEEK:
BATHING:
- You may shower the day after the procedure
- Do not soak in a bath for 72 hours
COMPRESSION:
- After showering, put on the compression hose. Compression will either be provided at the office or a prescription for hose will be given. The compression hose needs to be worn continuously (including at night) for the next 24 hours.
- For the following 2 weeks wear the compression stockings during the day
- You are strongly encouraged to walk for atleast 20 minutes every day
ACTIVITY & EXERCISE
- It is important that you walk for at least 20 minutes per day after this procedure, although an hour per day is preferred
- Light exercise like bike riding or gentle aerobics are safe options after 48 hours
- Vigorous exercises, bearing down, squatting, heavy weightlifting (>40LB) should be avoided for one week
PAIN:
- Manageable amounts of tenderness, bruising, and inflammation is expected after this procedure. These symptoms can be safely relieved with the use of over the counter ibuprofen (Advil), acetaminophen (Tylenol), and naproxen (Aleve).
- If the pain is not controlled by analgesics, please call Pioneer Heart Vein Center
DRESSING:
- The ACE and cotton dressing may be removed the next day
- You should expect noticeable bruising in the area of the phlebectomy sites
- You will see steri-strip tapes over the incisions. If they become displaced, you can replace them with an ordinary Band-Aid. If not, please leave the steri-strips in place for 7 days.
- You may notice some oozing of small amounts of blood after you remove the dressing – especially if you shower. This will stop with elevation of the leg and a short period of pressure over the site.
FOLLOW UP:
- You will come in within a week of each procedure (Usually 2 to 3 days) for an ultrasound and wound check
- After your final procedure, we will ask you to come in for a follow up appointment around six weeks later
IMMEDIATELY CALL PIONEER VEIN CENTER OFFICE IF YOU EXPERIENCE:
- Warmth or redness along the treated portion
- Fever over 101ºF
- Prolonged tenderness
- Shortness of breath
- Swelling in the treated limb
- Moderate or severe pain that stop you from performing normal activities
- Bleeding that cannot be controlled with moderate pressure
- Please also feel free to call with any other questions or concerns

